Savitri’s Director, Maggie Gardner, reflects on her recent visit to Uttar Pradesh, meeting families being supported by our recent programme partner, Emmanuel Hospital Association. Photos by Sunhil Sippy.
Our work on eyesight is a no brainer. Poor people who are blind through cataracts have an operation costing just £20 and they can see again. Older people regain their lives – can see to eat, wash, go to the loo, tend their fields, help with grandkids. Younger people can go back to work, and children to school often for the first time.
It’s amazing, joyous work.
I’ve just returned from India where I visited Savitri supported palliative care work – care for people who are dying.
I was shocked however, on my return to the UK to be asked by some people – not the majority – ‘why bother? Aren’t there bigger problems in India?’
I could use the economic response that decent access to palliative care saves families from debt. Middle income families pushed into poverty, people who are poor into taking out crippling loans they have no hope of repaying – resulting in some instances in kids being sold into bonded labour.
But having spent time with patients my more immediate, emotional response is we care for people who are dying, because we have compassion, because we are human, and in all honesty, because it saves people from horror.
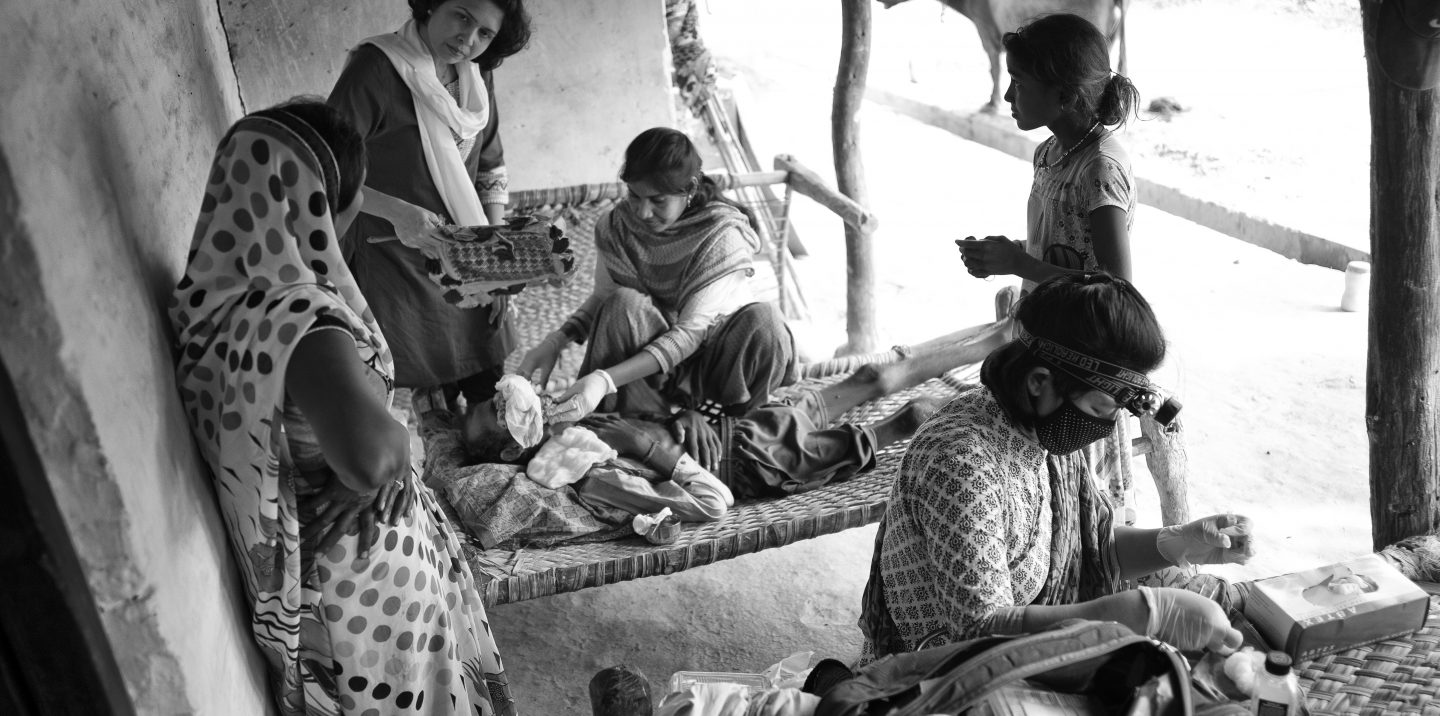
Just one example Mohan. He is 39 and now dead. But when I met him last week cancer had eaten away more than half of his face, covering his nose and eye with cauliflower shaped growths. The nurses picked out maggots and dressed his wound, while his 11-year-old daughter, Juli, bravely shone a light so they could see more clearly. His pain was controlled by morphine. His mum, wife and son looked on and were comforted and counselled by the EHA palliative care team.
The situation was bad but without the palliative care team there would be no morphine – no pain relief at all. No cleaning or dressing for the wound. No rehydration fluid. There would have been no training for the family in how to look after him. No touch – which he was able through the nurses to say was so important for him.
But more than that there would be no sweets – even in his last days Mohan was a man who knew what he liked, and he asked the nurses to bring sweets each time they visited (he also asked for extra sugar in his rehydration fluids). No comfort and support for the family – including helping them with the funeral and supporting them psychologically and practically as they deal with his death. No answer to his last wish which was to visit the hospital to say goodbye to the staff there who over the months of support had become his friends (we packed the family into the hospital car and all travelled together – a last good time for him, and a moment to remember for his family).
In India too often, people are just sent home from hospital to die. Without access to morphine or other pain killers, with families who are traumatised and don’t know how to look after loved ones who are very ill – they die in pain and without support.
Caring for people who are dying is a basic human response and helping people access care that is effective – brings I hope a kind of joy, the satisfaction of knowing you have helped.
Over the next few years Savitri plan to broaden our experience of palliative care in India. To learn and to share learning with others. To do what we can to push for decent medicinal access to morphine (The World Health Organization considers oral morphine, the cornerstone of cancer pain treatment), to support the amazing teams on the ground providing care, and to leverage additional support. We want to help make a difference.
In October 2017 a report in the Lancet said ‘The lack of global access to pain relief and palliative care …constitutes a global crisis, and action to close this divide between rich and poor is a moral, health, and ethical imperative. The need for palliative care and pain relief has been largely ignored.’
For me – as with eyesight Savitri’s work on palliative care is a no brainer.
Good to know if you agree.